Overview
The aim of the UGME program is to provide students with a general professional education as physicians. The program enables students to build upon previous education and experience, using available learning resources and opportunities. The competencies achieved by graduates will qualify them to proceed to further postgraduate training.
Like most medical programs, the McMaster UGME Program is divided into pre-clinical and clinical phases. Pre-clinical spans the first 15 months of the UGME program. The pre-clinical program uses problem-based, self-directed approaches and incorporates early patient exposure. In pre-clinical, the focus is on learning core medical science concepts and professional competencies to prepare students for the clinical program and beyond. The Medical Foundation (MF) tutorials and large group sessions present the major concept themes in the curriculum integrating the basic medical sciences. Anatomy and clinical skills sessions complement the MF material.
The tutorial group of 6-8 students is the key setting in which students will contribute to each other’s education under the guidance of a tutor. Students take responsibility for their own learning and time is allowed for independent, self-directed learning. There is a continuing assessment process including assessment by tutors, peers, and self, as well as program-related assessment exercises. Much of the curriculum is mounted electronically on MedPortal, the UGME program’s electronic platform.
The 63-week clinical program consists of rotations in medicine, general surgery, orthopedic surgery, family medicine, anesthesia, psychiatry, pediatrics, obstetrics and gynecology, and emergency medicine. There is also elective time, one-half of which must be spent in clinical activity. The compulsory components of the clerkship are carried out in teaching practices and in all the teaching hospitals in the regions of each campus: Waterloo, Niagara, and Hamilton. As well, many clinical placements occur in the communities associated with the Rural Ontario Medical Program.
Curriculum
Expandable List
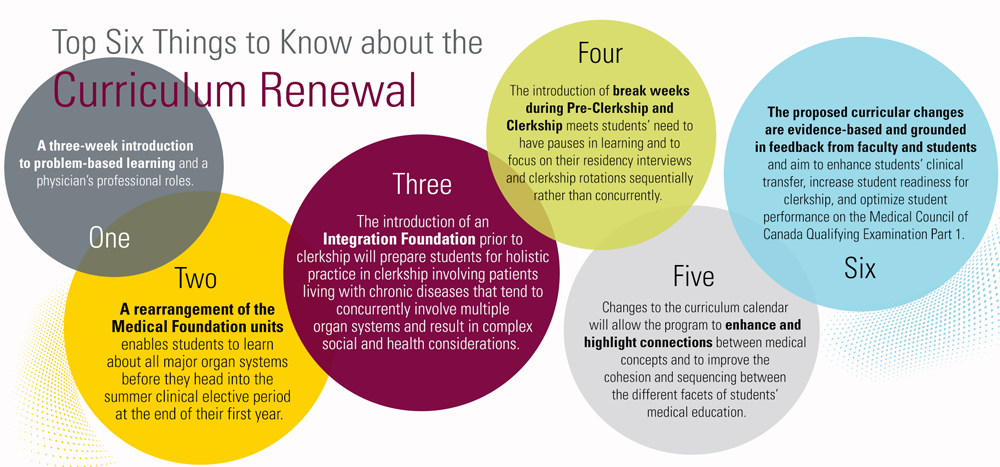
In 2019, the Undergraduate Medical Education program (UGME) undertook an extensive curriculum renewal, the culmination of a multi-year process that responded to feedback and experiences of its faculty and students, much of which reflects broader changes in healthcare research and medical education systems, and the professional responsibilities that physicians fulfill.
What are the advantages of a 3-week introduction to problem-based learning?
- A sustained orientation to PBL reaffirms the Michael G. DeGroote School of Medicine’s commitment to a pedagogy of PBL and deliberately introduces students to the rationale behind and process of PBL. Likewise, an introduction to the UGME graduating competencies prepares students for the breadth that their professional role will encompass.
What are the advantages of learning about all major organ systems before the summer electives?
- Most students participate in generalist electives or electives focused on diverse fields of medical practice and require knowledge and skills that are essential to having an optimal clinical learning experience. Students have indicated a strong preference to learn about all major organ systems before entering the summer elective that is scheduled at the end of their first year. Learning about all major organ systems benefits all students as they head into the summer elective and creates an opportunity for integration towards the end of pre-clerkship.
What are the advantages of the Integration Foundation?
- Healthcare in high-resource health systems is focusing increasingly on the care of patients living with chronic diseases that tend to concurrently involve multiple organ systems and result in complex social and health considerations. Medical curricula tend to focus on acute disease presentations to the neglect of chronic and complex diseases or health conditions. The Integration Foundation enables better coverage of complex and chronic health conditions, supports students’ integration of multiple aspects of medical practice in preparation for clerkship, and provides a structural mechanism for the repetition of key concepts. By concluding pre-clerkship with a unit that addresses complex and chronic care, students are impelled to review the major organ systems, which both consolidate medical concepts and skills while simultaneously preparing students for clerkship.
What are the advantages of break weeks?
- Mental health and well-being have been receiving increased focus in medicine for many years. McMaster’s UGME Program stands out as one of only two three-year MD degree programs in North America. The introduction of break weeks during Pre-Clerkship and Clerkship can easily be accommodated by the weeks introduced for an extended orientation, and these break weeks meet students’ need to have pauses in learning and to focus on their residency interviews and clerkship rotations sequentially rather than concurrently.
The small group Problem-Based Learning (PBL) tutorial is the cornerstone of the Pre-clerkship curriculum. Twice weekly, students meet in small groups with a faculty facilitator to study clinical problem scenarios. Each of the problem scenarios is accompanied by learning objectives that explore the connections between basic, applied, and clinical sciences with patient care concepts interwoven through the guided discovery of the problem scenario. Embedded questions within the cases introduce multiple opportunities for retrieval-based practice, which employ well-established blocked, spaced, and interleaved presentation techniques. Road maps are included with each tutorial problem scenario describing how the foundation and tutorial objectives are connected to previously learned topics, future learning, and the UGME Graduating Competencies representing the range of knowledge, skills, attitudes, and behaviours required to earn an MD degree at McMaster. The care of individuals with medical illness is emphasized in the tutorial problems with a particular focus on health equity and the social determinant of health. Tutorial problems stimulate students to integrate biomedical knowledge while considering the importance of the physical environment, access to health services, income, social status, childhood experiences, and social support. Between tutorials, large group teaching sessions with expert faculty employ active learning pedagogy to consolidate and review concepts introduced in tutorials.
Many students accepted into the UGME at McMaster have little or no experience with PBL. The first unit of the Pre-Clerkship curriculum called Introduction to Medicine deliberately introduces students to the rationale and process of PBL and transitions learners in the PBL environment on a more equal footing with the skills to benefit more fully from the advantages of a PBL curriculum. Each Medical Foundation in the Pre-Clerkship is integrated to promote the retention of knowledge and acquisition of skills through deliberate pre-programmed redundancy with progressively increasing complexity in the presentation of concepts and their application. Spiral integration throughout the Pre-Clerkship curriculum helps medical students more effectively build, consolidate, and integrate their knowledge and skills increasing student readiness for the next stage of learning in the clerkships and positioning graduates with the capability to provide responsive and dynamic patient-centered care as they continue on their professional journey.
The competencies outlined here represent the range of knowledge, skills, attitudes, and behaviours required to earn an MD degree at McMaster. They represent the foundations for generalist MD students who can enter any residency/post-graduate training program.
Patient Care
PROVIDE PATIENT-CENTERED CARE THAT IS COMPASSIONATE AND EFFECTIVE FOR THE TREATMENT OF HEALTH PROBLEMS AND THE PROMOTION OF HEALTH
- Gather essential and accurate information about patients and their health through history-taking, physical examination, and the use of laboratory data, imaging, and other tests.
- Organize and prioritize responsibilities to provide care that is safe, effective, and efficient
- Interpret laboratory data, imaging studies, and other tests required for the area of practice
- Make informed decisions about diagnostic and therapeutic interventions based on patient information and preferences, up-to-date scientific evidence, and clinical judgment
- Develop and carry out patient management plans
- Perform or assist with medical, diagnostic, and surgical procedures considered essential for the area of practice.
- Counsel and educate patients and their families to empower them to participate in their care and enable shared decision-making
- Provide appropriate referral of patients including ensuring continuity of care throughout transitions between providers or settings, and following up on patient progress and outcomes
- Provide health care services to patients, families, and communities aimed at preventing health problems or maintaining health
Knowledge for Practice
DEMONSTRATE KNOWLEDGE OF BIOMEDICAL, CLINICAL, EPIDEMIOLOGICAL, AND SOCIO-BEHAVIOURAL SCIENCES, AND APPLY THIS KNOWLEDGE TO PATIENT CARE
- Demonstrate an understanding of what knowledge is, the strengths and limitations of different ways of knowing, and how knowledge is created in historical, cultural, and social contexts
- Apply biomedical scientific principles fundamental to health care for patients and populations
- Apply principles of clinical sciences to diagnostic and therapeutic decision-making, clinical problem-solving, and other aspects of evidence-based healthcare
- Apply principles of epidemiological sciences to the identification of health problems, risk factors, treatment strategies, resource allocation, and disease prevention/health promotion efforts for patients and populations
- Apply principles of socio-behavioural sciences to the provision of patient care, including assessment of the impact of psychosocial and cultural influences on health, disease, care-seeking, care concordance, care adherence, and barriers to and attitudes toward care
- Understand the process of the dissemination, application, and translation of new health knowledge and practices
Practice-Based Learning and Improvement
DEMONSTRATE THE ABILITY TO INVESTIGATE AND EVALUATE ONE’S CARE OF PATIENTS, TO APPRAISE AND ASSIMILATE RESEARCH EVIDENCE, AND TO CONTINUOUSLY IMPROVE PATIENT CARE BASED ON REFLEXIVITY AND PRINCIPLES OF LIFE-LONG LEARNING
- Solicit and respond to feedback from peers, teachers, supervisors, patients, families, and members of healthcare teams regarding one’s knowledge, skills, attitudes, and professional behaviours
- Integrate feedback, external measures of performance, and reflective practices to identify strengths, deficiencies, and limits in one’s knowledge, skills, attitudes, and professional behaviours
- Set learning and improvement goals
- Identify and perform learning activities that address one’s gaps in knowledge, skills, and/or attitudes
- Understand principles of continuous quality improvement and how to incorporate them into practice improvement
- Locate, appraise, and incorporate evidence from research related to patients’ health problems and the provision of healthcare
- Use information technology and information systems to optimize patient care
- Obtain and use information about individual patients and their caregivers, populations of patients, or communities with which patients identify to improve care
- Continually identify, analyze, and implement new knowledge, guidelines, standards, technologies, products, or services that have been demonstrated to improve outcomes
Interpersonal and Communication Skills
DEMONSTRATE INTERPERSONAL AND COMMUNICATION SKILLS THAT RESULT IN THE EFFECTIVE EXCHANGE OF INFORMATION AND COLLABORATION WITH PATIENTS, THEIR FAMILIES, AND HEALTH PROFESSIONALS
- Communicate effectively with patients, families, and the public, as appropriate, across a broad range of socioeconomic and sociocultural backgrounds
- Participate in the education of patients, families, students, trainees, peers, and other health professionals
- Demonstrate sensitivity, honesty, and compassion in difficult conversations, including those about death, end of life, adverse events, bad news, disclosure of errors, and other sensitive topics
- Demonstrate insight and understanding about emotions and human responses to emotions that allow one to develop and manage interpersonal interactions, including the ability to manage one’s own interpersonal responses
- Maintain comprehensive, timely, and legible medical records
Professionalism
DEMONSTRATE A COMMITMENT TO CARRYING OUT PROFESSIONAL RESPONSIBILITIES AND AN ADHERENCE TO ETHICAL PRINCIPLES CONSISTENT WITH EXPECTATIONS OF SOCIETY, THE PROFESSION, AND LAW IN ALL PROFESSIONAL SETTINGS, INCLUDING CLINICAL, ACADEMIC, ADMINISTRATIVE, AND PERSONAL ACTIVITIES RELATING TO PROFESSIONAL PRACTICE
- Demonstrate accountability to patients, society, and the profession (PIP 1.3 (pdf))
- Demonstrate compassion, integrity, and respect for others (PIP 3.1 (pdf))
- Demonstrate altruism, appropriately balancing patient needs and self-interest/self-care (PIP 1.6 (pdf))
- Demonstrate respect for patient confidentiality, privacy, and autonomy (PIP 1.4 (pdf))
- Demonstrate sensitivity and responsiveness to a diverse patient population, including all dimensions of diversity such as those that are included in human rights legislation and federal and provincial law. (PIP 3.2 (pdf), PIP 3.4 (pdf))
- Demonstrate a critical understanding of personal, professional, and institutional power and privilege and utilize anti-oppressive practice to create patient experiences where marginalization and oppression are minimized.
- Demonstrate the application of ethical principles to commonly encountered ethical issues such as the provision or withholding of care, confidentiality, informed consent, and including compliance with relevant laws, policies, and regulations
- Balance personal values and beliefs with professional and societal ethics (PIP 1.6 (pdf))
- Maintain appropriate boundaries with patients and other professionals (PIP 3.3 (pdf))
- Manage conflicts of interest and dual relationships. (PIP 3.3 (pdf))
- Demonstrate trustworthiness and reliability that makes colleagues feel secure when one is responsible for the care of patients (PIP 1.1 (pdf), PIP 1.2 (pdf), PIP 1.3 (pdf))
- Present oneself professionally to patients, families, and members of the health care team (PIP 3.6 (pdf))
Systems-Based Practice
DEMONSTRATE AN AWARENESS OF AND RESPONSIVENESS TO THE LARGER CONTEXT AND SYSTEM OF HEALTH CARE, AS WELL AS THE ABILITY TO CALL EFFECTIVELY ON RESOURCES IN THE SYSTEM TO PROVIDE OPTIMAL HEALTH CARE
- Understand the systems of healthcare, including federal, provincial,
municipal and local, and the influences they have on the health of individuals and populations - Identify aspects of the healthcare system that serve as barriers and enablers of providing healthcare to and optimizing the health of patients and the population
- Advocate for quality patient care and optimal patient care systems that support patient- and population-centered care that is safe, timely, efficient, effective, and equitable
- Apply concepts of global health and social medicine to the health of individual patients and populations using the ecology, economy, and equity framework
- Work effectively in various healthcare delivery settings and systems relevant to a variety of clinical specialties
- Coordinate patient care within the health care system relevant to a variety of clinical specialties
- Incorporate cost, risk-benefit analysis, and resource stewardship inpatient and/or population-based care;
- Participate in identifying system-level gaps and errors and, where appropriate, identify, implement or participate in potential system-level solutions
- Perform administratively and practice management responsibilities commensurate with one’s role, abilities, and qualifications
Collaboration
DEMONSTRATE THE ABILITY TO ENGAGE IN INTER- AND INTRA-PROFESSIONAL TEAMS IN A MANNER THAT OPTIMIZES SAFE, EFFECTIVE PATIENT- AND POPULATION-CENTRED CARE
- Work with other health professionals to establish and maintain a climate of mutual respect, dignity, inclusion, ethical integrity, and trust
- Use the knowledge of one’s own role and the roles of other health professionals to appropriately assess and address the healthcare needs of the patients and populations served
- Communicate with other health professionals in a responsive and responsible manner that supports the maintenance of health and the provision of healthcare to individual patients and populations
- Demonstrate the ability to consult with and to other health professionals
- Work with physicians and other colleagues in the healthcare professions to promote understanding, manage differences, and resolve conflicts
- Participate in different team roles and appropriately apply leadership skills to establish, develop, and continuously enhance team function
Personal and Professional Development:
DEMONSTRATE THE QUALITIES REQUIRED TO SUSTAIN LIFELONG PERSONAL AND PROFESSIONAL GROWTH
- Demonstrate healthy coping mechanisms to respond to stress (PIP 3.5 (pdf)
- Practice flexibility and maturity in adjusting to change with the capacity to alter one’s behaviour
- Develop the ability to use self-awareness of knowledge, skills, and emotional limitation to seek help appropriately (PIP 2.2 (pdf), , PIP 2.4 (pdf))
- Demonstrate awareness and acceptance of different points of view (PIP 3.2 (pdf)
- Recognize that ambiguity is part of clinical health care and respond by utilizing appropriate resources in dealing with uncertainty
Pre-Clerkship
Expandable List
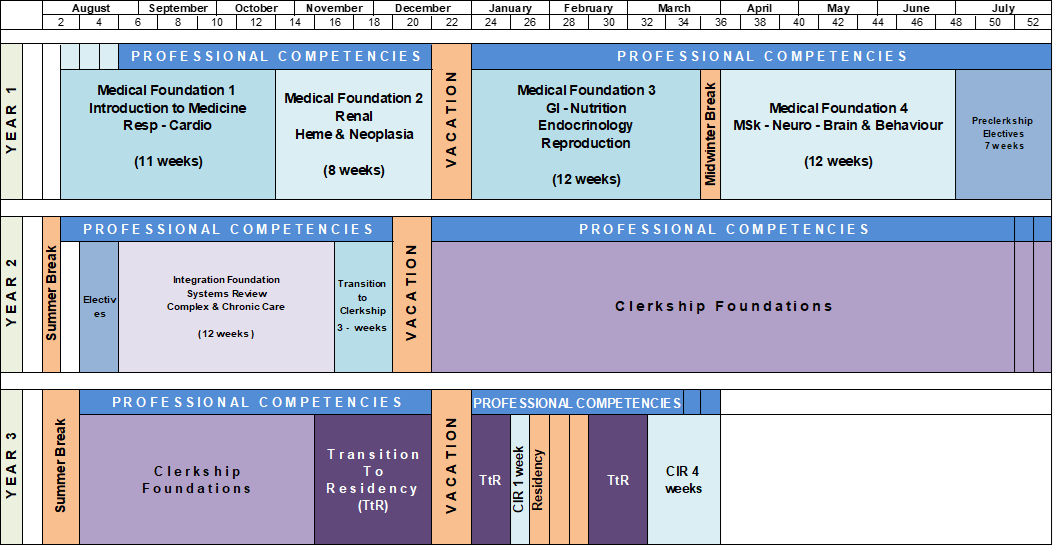
The Pre-Clinical curriculum is divided into five sequential Foundation units.
Small group problem-based learning is the core pedagogy in the pre-clinical MFs. During each MF, students are divided into tutorial groups of 6-8 students, with a faculty member acting as the tutor for the group. Tutorials take place twice each week, for about 3 hours each time. In addition to tutorials, students attend some Active Large Group Sessions as a class. Each group also has anatomy and clinical skills sessions.
MEDICAL FOUNDATION 1
- 11 weeks, August to October of first year. All students in their assigned campuses. Focus on introduction to medicine, respiratory, and cardiology.
MEDICAL FOUNDATION 2
- 8 weeks, October to December, finishing prior to the December holiday break. All students in their assigned campuses. Focus on renal and hematology.
MEDICAL FOUNDATION 3
- 12 weeks, January to March of first year, followed by a one-week winter break. All students in their assigned campuses. Focus on GI and Nutrition, Endocrinology, and Reproduction.
MEDICAL FOUNDATION 4
- 12 weeks, April to June of first year, followed by summer break, and then a 7-week block elective. All students in their assigned campuses. Focus on Musculoskeletal Medicine, Neuroscience, and Brain and Behaviour.
INTEGRATION FOUNDATION
- 12 weeks, August to November of second year. All students will review, revisit, and refresh previous learning content and objectives from MF1 to MF4 in the context of complex, multi-system diseases and chronic illness.
The Clinical Skills Program of the UGME Program is designed to allow students to develop an integrated approach to the doctor-patient encounter. The Program has three components: first, verbal data-gathering, which includes communication skills and history-taking; a second component of physical examination skills; and a third component, data interpretation, which rounds out the doctor-patient encounter. This component includes the interpretation of verbal and physical findings from the patient as well as diagnostic tests.
In most MFs, each MF tutorial group works with a clinical skills preceptor in weekly sessions focused on the clinical skills appropriate to the topics being covered in the MF. From the first MF, students begin meeting patients. There are also sessions with Standardized Patients, which allow students to master basic skills before they begin to use these skills with real patients.
The Clinical Skills curriculum and the Professional Competencies curriculum are closely linked in teaching students the basic communication skills so vital to good clinical practice.
As students progress, more specialized clinical skills such as those relating to psychiatric interviewing and ophthalmology are taught using varied formats.
Anatomy is a core foundation of the Pre-Clerkship curriculum and is taught in weekly lab sessions. These sessions involve a station-based, self-guided learning environment with models/protected specimens and pathological specimens available for learning. Faculty preceptors are present during these sessions to expand concepts and bring clinical relevance to the material. Radiology and imaging sessions are interspersed throughout the anatomy curriculum to further integrate fundamental anatomy with modalities for assessing anatomy in vivo.
Clerkship
The 63-week Clerkship program is an integral part of the UGME program and consists of three phases: Transition to Clerkship, Clerkship Foundations, and Transition to Residency.
The Transition to Clerkship period (3 weeks) was jointly developed and delivered through the collaboration of the Pre-Clerkship, Clinical Skills, and Professional Competencies teams. This phase will focus on: (a) practical skills sessions; (b) opportunities for in-depth orientation/introduction to specific clinical environments such as the operating room (e.g., “scrubbing in”), clinic, and ward; (c) review and practice of common practical skills; (d) opportunities to learn and/or practice objectives and skills currently taught in specific rotations; (e) opportunities to revisit and transition concepts introduced through the Clinical Skills and Professional Competencies curricula that are important for Clerkship.
The Clerkship Foundations phase (44 weeks) begins immediately after the three-week Transition to Clerkship phase. This phase includes 9 core rotations and 12 weeks of electives. There will be 7 core rotations that are 4 weeks in duration (Medicine, OB/Gyn, Surgery, Psychiatry, Pediatrics, Family Medicine, and Emergency Medicine). There will be 2 rotations that are 2 weeks in duration (Anesthesia and Orthopedics).
The Transition to Residency phase (16 weeks) will consist of 6 rotations of 2 weeks duration in: Medical Sub-Specialty Selectives, Internal Medicine, Pediatrics, Psychiatry, Surgery, and Family Medicine. Five of these rotations (all excluding MSS) will be “Plus Two” rotations allowing students to revisit rotations they experienced in the Clerkship Foundations phase. There will be a total of 4 weeks of electives in this phase with 2 weeks occurring prior to the 3-week residency interview period.
The compulsory components of the Clinical program are carried out in teaching practices and in all the teaching hospitals in the regions of each campus: Waterloo, Niagara, and Hamilton. As well, many clinical placements occur in the communities associated with the Rural Ontario Medical Program.
In the pre-clinical portion of the renewed curriculum, students will be better positioned to call upon and consolidate knowledge and skills during their clinical rotations. During the national residency interview period, students will be able to focus on interviews and clinical responsibilities consecutively rather than concurrently.
Expandable List
This is a 2-week rotation during which students are exposed to many concepts of anesthetic practice in a combination of small group sessions, problem-based learning, part-task, and full-body simulators, as well as multiple clinical environments.
The objectives are:
- To acquire an appreciation of the multifaceted discipline of Anesthesia
- To acquire an understanding of the clinical application of physiology and pharmacology to patients of all ages
- To acquire the basic practical skills of the airway and circulatory management
During this 4-week rotation, students will learn to:
- Demonstrate the ability to rapidly recognize and initiate basic management of acute life- or limb-threatening illness or injury
- Describe a basic differential diagnosis including the significant worst-case diagnosis for every patient assessed
- Demonstrate a basic systematic, prioritized approach to resuscitation and stabilization of emergencies
- Demonstrate a basic ability to distinguish seriously ill or injured patients from those with minor conditions
- Demonstrate a focused history and physical examination
- Distinguish which conditions are life-threatening or emergent from those that are less urgent
- Demonstrate the ability to evaluate and initiate treatment of the undifferentiated patient
- Describe the concept of triage and prioritization of care, including paraphrasing the use of CTAS. Recognize that certain groups of patients require a high index of suspicion for serious illness (e.g., immunocompromised, chronic renal failure, transplant, extremes of age, intoxicated, and diabetes)
The 4-week Family Medicine rotation revolves around a one-to-one experience pairing a student with a community-based family physician. The most significant component of the Family Medicine rotation is the time spent with the clinical preceptor in the office setting.
The overall goals of the program are for all students to have:
- An understanding of the broad scope of family medicine
- An understanding of how virtual or same-site interprofessional teams function in the context of the primary care environment
- Appreciate the challenges in addressing complex, diverse patient care issues longitudinally
- Appreciate the nature of some of the specific challenges in the provision of primary care to patients, such as addressing undifferentiated illness, chronic illnesses, and preventive care issues.
- Gain skills and experience in meeting patients’ needs for prevention, problem identification and management, and complex disease management through episodic care of patients and their families in the community practice setting
The cornerstone of the family medicine experience is the close relationship that learners develop with their preceptors when working together in the delivery of care to patients in the preceptor’s office, but also in other contexts such as long-term care, palliative care, and hospital settings.
Internal Medicine is a challenging and diverse specialty comprised of physicians who care for a broad range of adult patients with both acute and chronic conditions. They are also involved in health promotion and disease prevention. They treat a wide of conditions and provide compassionate care to a diverse group of patients. Internal Medicine physicians need to be experts in multiple domains including history and physical exam skills, diagnostics, therapeutics, communication, team interaction, interdisciplinary collaboration, and patient advocacy.
The Internal Medicine rotation consists of a 4-week core rotation, a 2-week transition to residency rotation, and a 2-week mandatory subspecialty selective rotation. The core rotation in Hamilton occurs at one of 3 hospital-based Clinical Teaching Units and there are also ward-based rotations at the hospitals associated with the Kitchener/Waterloo and Niagara campuses. The Internal Medicine clerkship objectives are a framework of basic competencies which are appropriate for mastery by clinical clerks during their rotation, and which include the content knowledge objectives.
Internal Medicine Clerkship Objectives are achieved in the following areas:
- History and Physical Examination
- Case Presentation
- Problem Formulation: Diagnosis
- Problem Formulation: Therapy
- Communication with patients
- Professionalism
- Bioethics of care
- Self-directed learning
- Basic Procedures
- Care of the Elderly
The Obstetrics and Gynecology rotation is a dynamic 4-week clinical rotation where learners are assigned to a hospital site. Students will participate in their specific site call schedule and will spend the majority of their time in Triage on the Labour and Delivery Ward (Although each site will have some differences).
Students will mainly be participating in approximately 12-hour shifts focused on care in triage at L&D wards. In some sites, additional time will be spent in clinics. This may differ depending on each individual site. Some of the learning you will obtain will be:
- Labour assessments
- Fundal heights
- Fetal heart monitoring
- Reviewing antenatal records
- Dealing with pregnancy-related illnesses
- speculum exams (if ruptured membranes)
The Orthopedic Surgery core is a 2-week rotation.
Students become familiar with the following areas (and when applicable with the signs, symptoms, relevant investigations, treatments, and prognosis) of:
- Fractures and dislocations.
- Painful and/or swollen joints.
- Limb deformity (Paediatric/malunion)
- Inflammatory and non-inflammatory arthritis.
- Musculoskeletal tumors.
- Cervical/low back pain and sciatica
The pediatrics clerkship is split into a 4-week “core” rotation and 2 weeks of “transition to residency” pediatrics (TTR). During Core Pediatrics, students have exposure to ambulatory and inpatient pediatrics care. The student experience focuses on well children, acute medicine, and chronic/complex diseases. Education about common pediatric clinical presentations, health maintenance, and disease prevention are reviewed along with pediatric clinical skills training focused on interviewing, examination, and clinical management. The 2-week “transition to residency pediatrics experience is a mix of general pediatrics and subspecialty clinics, aimed at fine-tuning knowledge and building higher-level clinical skills.
The Psychiatry clerkship rotation is split into two rotations – a full-time four-week foundation rotation during which students are exposed to various psychiatric patients and settings and a two-week Transition to Residency rotation that allows students to build on the skills they developed during their foundational rotation. The rotation is comprised of several components including a clinical placement (options of community, inpatient, outpatient, and specialty areas), a Psychiatry emergency room on-call experience, and a mandatory academic half day which includes teaching and tutorial sessions of various formats. Clinical placements may be in Hamilton, Waterloo, Brampton, Niagara region, or surrounding community settings (e.g. Burlington, Oakville).
This is a 4-week rotation during which students are involved in a variety of clinical scenarios and learning opportunities designed to enhance their knowledge and skills. They interact with patients and their families in all aspects of surgical care (hospital wards, outpatient clinics, operating rooms, emergency departments, intensive care units, etc.). They are part of a team of highly qualified physicians and other healthcare professionals.
The aim of the surgical clerkship is for the students to achieve a defined body of knowledge, skills, and attitudes necessary for the recognition and understanding of the management of patients with diseases that may be treated by surgeons. This clerkship will provide the foundation necessary for the student to enter into any field of medical practice.?
CONCEPT INTEGRATION AND REVIEW (CIR)
This is a 5-week block in 3rd year, after Clerkship ends and just before the students graduate and write their MCCQE Part 1 licensing exam.
The purposes of the unit:
- To help students review and synthesize important concepts;
- To provide an opportunity for students to practice answering multiple choice and key-features questions before the MCCQE Part 1 exam;
- To review some presentations that might challenge students as new residents.
As a consequence of the changes being proposed in the curriculum renewal process, students will more likely enter the CIR block feeling that their knowledge and skills are consolidating and that they feel well-prepared to write the Taken collectively, the curricular changes aim to help medical students more effectively build, consolidate, and integrate their knowledge and skills, thus offering an opportunity to measurably enhance students’ clinical transfer of concepts introduced in the pre-clinical curriculum, increase student readiness for clerkship, and improve student performance on high stakes summative examinations such as the Medical Council of Canada Qualifying Examination Part 1, thereby positioning graduates with the capability to provide responsive and dynamic patient-centered care as they continue on their professional journeys.
Professional Competencies
The Professional Competencies curriculum is interwoven throughout the 3-year program. This component of the curriculum enables the student to pull together the complexities of clinical practice: ethics, communication skills, self-reflection, health systems, interprofessional teamwork, and more. These make up the layers of meaning and being that well-rounded doctors of tomorrow must possess. Clinical skills will be introduced early and often, a hallmark of McMaster’s patient-centered curriculum. Patient partners and more hands-on clinics – as well as enhanced resources in the clinical learning center – round out the offerings.
This curriculum is anchored by a weekly tutorial session led by an MD and an allied health professional who will remain with their group throughout 15 months of pre-clerkship.
In addition to this, the Professional Competencies stream will be purposefully integrated with the Medical and Integration Foundations tutorial sessions, Clinical Skills, and Clerkship. In the renewed curriculum, students will approach their first Professional Competencies discussion with a stronger grounding in the professional expectations of a physician. As they progress through their first year, students will notice congruency between the theoretical discussions that they are having in Professional Competencies groups and the simulated practice they undertake in Clinical Skills labs.
KEY DOMAINS
The Professional Competencies stream is a competency-based, longitudinal curriculum with a focus on seven key domains:
Expandable List
Upon completion of the Undergraduate Medical Program, the medical student will be able to competently:
- Illustrate how being a good communicator is a core clinical skill for physicians, and how effective physician-patient communication can foster patient satisfaction, physician satisfaction, adherence, and improved clinical outcomes (CanMEDS 2015).
- Demonstrate how to perform the basic communication and interpersonal skills that are required to accomplish each of the specific and discrete tasks defined in the Kalamazoo Consensus Statements. (1999, 2002).
- Demonstrate the specific skills for interacting with and responding to patients who present moderate communication challenges (anger; anxiety; values different from the students’ own).
- Demonstrate how to develop with patients, families, and other professionals a common understanding of issues and a shared plan of care, as defined by the Kalamazoo Consensus Statements. (CanMEDS 2015).
- Demonstrate how to communicate orally, in written form, and via information databases when collaborating as a member of a multidisciplinary healthcare team on the health of a patient.
- Demonstrate how to communicate about medicine and science in a variety of contexts and appropriately for the given audience, setting, and information being presented.
- Summarize the concepts, principles, and research evidence that support the importance and efficacy of developing communication and interpersonal skills in medicine.
- Demonstrate the acquisition of communications skills (defined by the Kalamazoo Consensus Statements as a set of conscious and behavioural norms) required to build a therapeutic relationship, conduct an interview with a patient, communicate about a patient, and communicate about medicine and science.
Upon completion of the Undergraduate Medical Program, the medical student will be able to competently:
- Identify personal limitations in knowledge and pursue the information needed to understand problems and make decisions both in patient care and at the population level.
- Search for and organize essential and accurate research evidence.
- Appraise, incorporate principles of resource stewardship to, and apply acquired knowledge into medical decision-making.
- Incorporate patient, inter-professional team, and system factors into medical decision-making.
- Demonstrate active planning for the pursuit of knowledge and lifelong learning to maintain competency.
- Apply principles of evidence-based and evidence-informed medicine in medical decision-making.
- Demonstrate how to engage in shared decision-making with a patient, group, community, or population.
- Assess the use of narrative in the process of meaning-making, both for patients and clinicians.
Upon completion of the Undergraduate Medical Program, the medical student will be able to competently:
- Describe how individuals develop a capacity for moral thought and how personal values impact moral reasoning.
- Employ and critically evaluate ethical theories and principles when exploring learning scenarios and reasoning about ethical challenges in the clinical setting.
- Judge when additional expertise is needed in the resolution of ethical choices and where to find appropriate resources (help, laws, policies, etc.) to obtain this help.
- Apply the McMaster framework for moral reasoning.
- Identify ethical issues and dilemmas in their own clinical experiences related to patient care, institutional practices, and health policies.
- Demonstrate sensitivity to the value system of patients (colleagues, other health care providers – ethical vs professionalism) and others.
- Summarize the ethical and legal obligations, and duty of care that physicians have for patients, colleagues, and communities, and the tensions that may arise from these responsibilities.
- Integrate moral reasoning and judgment with communication, interpersonal, and clinical skills to provide patients with effective and ethical care.
- Describe the mechanisms for system improvement, including responsible reporting, whistleblowing, and internal and external approaches.
- Demonstrate awareness of how social contexts and epistemological perspectives, such as privilege and power, contribute to uncertainty and ethical challenges in practice.
Upon completion of the Undergraduate Medical Program, the medical student will be able to competently:
- Define and discuss concepts of health, wellness, illness, disease, and sickness (including WHO and Health Canada definitions, Lalond Report, Ottawa Charter for Health Promotion).
- Know how to access and collect health information to describe the health status of a population.
- Describe the types of data and common components (both quantitative and qualitative) used in creating a community needs assessment.
- Describe the determinants of health and how the differential distribution of these determinants influences health status (health gradient) both within and between populations.
- Illustrate how diverse factors (sociocultural, psychological, economic, occupational, environmental, legal, political, spiritual, and technological) interact to influence the health of an individual and the population.
- Plan and advocate for an appropriate course of action at both the individual- and population levels that responds to the diverse factors influencing their health.
- Describe approaches and challenges to working with different vulnerable populations to improve their health. (ex. people experiencing homelessness; people at extremes of the age continuum).
- Identify the ways in which health systems (federal, provincial, municipal, private, non-governmental) can address structural barriers to reduce inequities in health status between population groups.
- Describe the role that physicians can play in promoting health and preventing diseases at the individual and population levels.
- Describe the professional responsibility of the physician as a Health Advocate in advancing the health and well-being of individuals, communities, and populations.
- Understand how public policy can influence community-wide patterns of behaviour and affect the health of a population.
Upon completion of the Undergraduate Medical Program, the medical student will be able to competently:
- Describe professionalism as it applies to medical student practice, including formal education and clinical experiences and informal functioning within the Faculty of Health Sciences.
- Illustrate strategies to cope adaptively with stresses likely to occur during medical training and practice.
- Employ value constructs foundational to the practice of medicine and the delivery of health care, including constructs related to vulnerable and marginalized populations and to the recognition of cultural diversity (using a broad definition and understanding of culture).
- Contrast organizational structures applied within institutions and agencies accountable for the delivery of health care.
- Employ strategies for successful team functioning as they apply to various learning environments.
- Demonstrate skills in negotiation and conflict resolution.
- Describe the range and scope of contemporary medical practice as well as the role of the physician in emerging healthcare models.
- Demonstrate management of practice environments, including charting, public reporting expectations, and malpractice risks.
- Demonstrate appropriate behaviours, habits, and skills required for referral and consultation.
- Apply standards of care, institutional policies, and standard operating procedures.
- Recognize personal strengths and limitations relevant to one’s practice of medicine.
- Understand the importance and impact of interpersonal interactions in both professional and personal settings.
- Integrate and apply performance and interpersonal feedback as part of training and practice.
- Identify and address problems/issues that might affect one’s own health, well-being, or professional capabilities.
Upon completion of the Undergraduate Medical Program, the medical student will be able to competently:
- Demonstrate skills for critical intersectional analysis.
- Justify how knowledge from the social sciences and humanities contributes to medical practice.
- Summarize different “ways of knowing” about the body and how these ways affect the clinical encounter.
- Illustrate the difference between disease and illness, and plan an approach to understanding the patient’s illness experience.
- Analyze and critically reflect on how the impact of physician power and privilege may contribute to disparities through biased care.
- Develop the attitude and skills for responding to patients with cultural humility.
- Analyze the influence of gender on health concerns and healthcare provision.
- Discuss the historical and contemporary events and the systemic factors influencing current practices and issues regarding Indigenous Health and anti-Indigenous racism, all of which impact current and future practitioners, individuals, and communities.
- Identify opportunities to educate and reflect on events of Indigenous self-determination, cultural preservation, and growth to foster allyship in Indigenous Healthcare and community settings.
- Demonstrate an awareness of key health challenges faced by immigrants and refugees.
- Recommend responses to key social and cultural factors that lead to poor health outcomes for individuals, families, and communities.
- Identify the diverse factors (ie. sociocultural, psychological, institutional, economic, occupational, environmental, technological, legal, political, and spiritual) that contribute to the systemic marginalization of vulnerable populations and impact health and health care delivery.
- Plan socially-just courses of action in order to respond to the diverse factors that intersect and overlap to influence the health of individuals, families, and communities.
Upon completion of the Undergraduate Medical Program, the medical student will be able to competently:
- Contrast a physician’s professional roles, responsibilities, and scope of practice with the respective professional roles, responsibilities, and scopes of practice of other health professionals.
- Judge when and how to involve or consult other health professionals in patient care, as appropriate to a health professional’s roles, responsibilities, scope, and competence.
- Demonstrate strategies for establishing common goals, continuity of care, and a climate for collaborative practice amongst all participating health professionals in the course of providing care to individuals and their caregivers.
- Demonstrate strategies that facilitate appreciation of differences, shared decision-making, and conflict resolution amongst all participating health professionals in the course of providing care to individuals and their caregivers.
- Illustrate how a physician’s language and behaviour can facilitate interdependent, appreciative, and trusting working relationships amongst a team of health professionals.
- Demonstrate methods for seeking from and offering to other health professionals feedback that improves the knowledge, work processes, and outcomes of a team of health professionals.
- Exhibits a consistent commitment to valuing the expertise, perspectives, co-leadership, and dignity of other health professionals.
- Demonstrate their capacity to function within inter-professional teams.
Electives
Elective studies form an integral part of the Curriculum Plan. They may be considered the epitome of self-directed learning since students must define goals for electives that are appropriate for their own learning objectives. These objectives represent specific areas of educational need, career exploration, or interest.
Expandable List
Block electives are full-time elective placements. Over the course of the program, 24 weeks of block electives are required. The first block elective occurs after MF4, in the summer between first and second year. Students participate in 7 weeks of electives during that block. In the Clerkship, 17 weeks of elective time is available.
The Family Medicine Experience (FME) is an optional elective rotation during Pre-Clerkship in which students have clinical, in-person contact with patients in order to practice clinical skills in an observed, primary care clinical setting. The FME runs for 12 hours over two full days or three to four half-days.
Horizontal Electives are entirely optional observership or shadowing experiences undertaken concurrently with other parts of the curriculum. Horizontal electives are not required for completion of the UGME curriculum.
Horizontal Research Electives are entirely optional research opportunities undertaken concurrently with other parts of the curriculum in order to strengthen critical thinking, research, and learning skills. Horizontal research electives are not required for the completion of the UGME curriculum.
Pre-Clerkship Electives are mandatory blocks of curriculum time dedicated to full-time elective activities.
Clerkship Electives are mandatory blocks of curriculum time that allow students to hone their skills in exploring a variety of clinical areas and dedicating time to research.
Reading Electives are an optional means of completing an elective while still allowing students to explore areas of interest in greater depth through directed reading under the guidance of a preceptor.
Research Electives are an optional means of completing an elective while still allowing students to explore areas of interest in greater depth through directed research under the guidance of a preceptor.
Visiting electives are Clerkship block electives secured via the AFMC Student Portal and completed at other Canadian medical schools. Visiting electives are subject to the parameters (i.e. duration, expectations, supervision) of Clerkship block electives.
International electives are Pre-Clerkship or Clerkship block electives completed outside of Canada. International Electives are required to be at least four weeks in duration to ensure that the student is receiving a valuable learning experience abroad. International electives are subject to the parameters (i.e. duration, expectations, supervision) of the clinical block elective being replaced.
Required Documents
Expandable List
This is only for students who have confirmed electives.
In order to obtain computer access at HHSC sites, you are required to complete and submit a Confidentiality Agreement Form (CAF) through the AFMC portal.
Students will be contacted regarding mandatory computer access training session prior to the start of their elective.
Students with a home school in Canada are required to accurately list all prior addresses they have resided in for more than six months consecutively for the past five years prior to their elective start date on their Vulnerable Sector Check application.
When applying for a visiting elective, students must upload a pdf of their Vulnerable Sector Check with their application on the Association of Faculties of Medicine of Canada (AFMC) portal. Failure to upload this documentation may result in delayed processing of an elective application or a cancelled elective.
It is recognized that similar documentation may be a requirement of the student’s home university therefore, VSCs must be issued with McMaster University or the student’s home school listed as the requesting agency.
Vulnerable Sector Screens must be issued within 12 months of the end date of the elective. If a student’s current VSC or Police Certificate will expire before or during the elective, the student may submit their current document with their application but must, at least 8 weeks prior to the elective start date, upload a new VSC or Police Certificate which is valid until the end of the elective.
Visiting Elective students must make readily available the original copies of uploaded VSCs and/or Police Certificates as they can be requested for verification by the Michael G. DeGroote School of Medicine, the FHS Professionalism Office or the clinical site when attending an elective. Failure to produce original copies when requested may result in a cancelled elective
For Toronto Police Record Requests: an original copy of the “Consent to Disclosure of Personal Information” form is required when requesting a Vulnerable Sector Screen (VSS) from Toronto Police Services. Once your elective is confirmed please email fhsprof@mcmaster.ca with your full name, AFMC application number and your Toronto home address so that a form can be mailed to you. In the interim, a previous police check or letter stating your intent to obtain a Toronto VSS should be uploaded with your application.
-
International students (which includes Canadian citizens who are studying abroad) are required to provide a Police Certificate from each country or territory that they have resided in for more than six months consecutively for the past five years prior to their elective start date.
-
Police Certificates must be issued within 12 months of the end date of the elective. If a student’s current Police Certificate will expire before or during the elective, the student may submit their current document with their application but must, at least 8 weeks prior to the elective start date, upload a new Police Certificate which is valid until the end of the elective.
-
Once the police record check is obtained, the document must be scanned and uploaded onto the AFMC portal.
Failure to submit the police record check may result in the AFMC application not being processed.
Visiting Elective students must make readily available the original copies of uploaded Police Certificates as they can be requested for verification by the Michael G. DeGroote School of Medicine, the FHS Professionalism Office or the clinical site when attending an elective. Failure to produce original copies when requested may result in a cancelled elective.
For Toronto Police Record Requests: an original copy of the “Consent to Disclosure of Personal Information” form is required when requesting a Vulnerable Sector Screen (VSS) from Toronto Police Services. Once your elective is confirmed please email fhsprof@mcmaster.ca with your full name, AFMC application number and your Toronto home address so that a form can be mailed to you. In the interim, a previous police check or letter stating your intent to obtain a Toronto VSS should be uploaded with your application.