At a Glance
MEDICINE AT McMaster
The School of Medicine, established in 1965 and renamed the Michael G. DeGroote School of Medicine in 2004, offers major programs in undergraduate, postgraduate, and graduate medical education. The clinical programs use not only the teaching hospitals and ambulatory care and research facilities, but also the clinical teaching units at several of the major hospitals and community healthcare centers.
The Undergraduate Medical Education program for the MD degree was initiated in 1969, graduating its first students in May 1972. At present, 203 students are admitted to the program each year.
The three-year program in Medicine uses a problem-based approach to learning that should apply throughout the physician’s career. The components have been organized in sequential blocks with early exposure to patients and case management. The academic program operates on an 11 months-a-year basis and students qualify for the MD degree at the end of the third academic year.
Expandable List
To achieve the objectives of the medical program, students are introduced to patients within the first Foundation of the curriculum. In this way, students understand the relevance of what they are learning, maintain a high degree of motivation and begin to understand the importance of responsible professional attitudes. Students are presented with a series of tutorial problems, requiring their explanation, the understanding of underlying biological, population, and behavioural principles, the appropriate collection of data, and the critical appraisal of evidence. The faculty function as learning resources or guides. Learning by a process of inquiry is stressed.
The central focus of the program is the tutorial. The class is divided into small groups, each with a tutor. In the tutorial, session students develop a series of learning objectives from each healthcare problem and negotiate how they will approach their learning tasks. They then acquire the knowledge and skills to meet the objectives of the Foundation in which they are working. They also learn to work as a team, helping and learning from peers. The study habits and sense of responsibility to self and others provide a basis for lifelong learning.
Some of the advantages of PBL are: early exposure to the clinical settings and patients; the motivation to learn is self-imposed; students can see the practical application of the knowledge they are acquiring during their studies, and the acquisition of various learning skills promotes lifelong learning.
The Michael G. DeGroote School of Medicine fosters a cooperative, supportive and respectful environment. The curriculum evolves continuously, responsive to the challenging needs of Ontario society, nurturing the development of the following competencies at the time of graduation:
- Patient Care: Provide patient-centered care that is compassionate and effective for the treatment of health problems and the promotion of health;
- Knowledge for Practice: Demonstrate knowledge of biomedical, clinical, epidemiological, and socio-behavioural sciences, and apply this knowledge to patient care;
- Practice-Based Learning and Improvement: Demonstrate the ability to investigate and evaluate one’s care of patients, to appraise and assimilate research evidence, and to continuously improve patient care based on reflexivity and principles of life-long learning;
- Interpersonal and Communication Skills: Demonstrate interpersonal and communication skills that result in the effective exchange of information and collaboration with patients, their families, and health professionals;
- Professionalism: Demonstrate a commitment to carrying out professional responsibilities and an adherence to ethical principles consistent with expectations of society, the profession, and law in all professional settings, including clinical, academic, administrative, and personal activities relating to professional practice;
- Systems-Based Practice: Demonstrate an awareness of and responsiveness to the larger context and system of health care, as well as the ability to call effectively on resources in the system to provide optimal health care;
Collaboration: Demonstrate the ability to engage in inter- and intra-professional teams in a manner that optimizes safe, effective patient- and population-centered care; - Personal and Professional Development: Demonstrate the qualities required to sustain lifelong personal and professional growth.
Mission: Together advancing health through learning and discovery.
The COMPASS curriculum focuses on the mastery of fundamental concepts in medicine and aims to endure that our graduates have a good working understanding of biological, psychological, and social mechanisms and processes, as well as their impact on health and disease, based on principles of learning drawn from cognitive psychology. The COMPASS curriculum is structured to allow the integration of critically important fundamental concepts in medicine and affords an opportunity for students to have the time to practice applying these concepts to multiple different clinical problems.
The pre-clerkship is divided into five Foundations as well as a horizontal Professional Competencies curriculum which runs throughout the three years of the program.
- Medical Foundation 1 begins with a three-week Introduction to Medicine, which introduces students to areas of personal and professional development required to study medicine as well as the pedagogies and assessments that are employed in the Program. This block is followed by two four-week subunits, one focusing on core concepts related to respiratory and the second focusing on cardiology.
- Medical Foundation 2 focuses on the renal and hematologic systems’ contribution to concepts of oxygenation and homeostasis. Immunologic and host defense aspects of hematology are addressed and students are introduced to some basic concepts in neoplasia.
- Medical Foundation 3 focuses on concepts of nutrition, energy, homeostasis, and reproduction through the study of the digestive, endocrine, and reproductive systems.
- Medical Foundation 4 focuses on concepts of locomotion and neurosensory and behavioural responses to the environment. Students explore the musculoskeletal system, the neurological system, and psychiatric medicine.
- The final unit in the Pre-Clerkship is the Integration Foundation. This Foundation focuses on a review of key concepts from the four Medical Foundations in the context of complex, multi-system diseases, chronic illness, immunology, host defense, neoplasia, maternal and child health risks, and aging-related health care. The Integration Foundation allows students to consolidate medical concepts and skills, clinical skills, and professional competencies, readying them for the transition to Clerkship.
- The Clerkship program consists of rotations in medicine, surgery, family medicine, anesthesia, psychiatry, pediatrics, obstetrics and gynecology, emergency medicine, and electives. Teaching is carried out in clinical practices and in all the teaching hospitals in the Hamilton, Waterloo, and Niagara Regions. Students are expected to travel outside of their home campus area for clerkship rotations and are responsible for transportation and associated costs in order to complete rotation requirements.
Integral to our mission are our extensive research programs. McMaster has been Canada’s top research-intensive university for the past three years, and the Faculty of Health Sciences is a major contributor to this success.
The curriculum at all three campuses is identical and takes full advantage of videoconferencing technology to ensure parallel experiences at each of our campuses.
McMaster’s Hamilton campus, which is restricted to pedestrian traffic, is adjacent to the Royal Botanical Gardens at the western end of Lake Ontario. The campus is minutes from downtown Hamilton and the activities that a major city has to offer. Clinical placements are conducted in local hospitals and outpatient clinics as well as community physician’s offices in the surrounding areas including Guelph, Oakville, Burlington, Brantford, Dundas, Ancaster, Stoney Creek, Newmarket, and Mississauga.
The Niagara Regional Campus was planned for students who wish to learn and experience medicine with the benefit of a regional campus setting. The academic portion of the program is delivered at the Cairns Family Health and Bioscience Research Complex at Brock University in St. Catharines, Ontario. Practical hospital experience occurs at the seven sites in the Niagara region and is taught by exceptional local physicians. Clinical placements are provided in outpatient clinics, private offices in various specialties, the Public Health Unit, the Niagara Health System sites, Hotel Dieu Shaver Health and Rehabilitation Centre, and West Lincoln Memorial Hospital in Grimsby.
The Waterloo Regional Campus is located in the University of Waterloo Health Sciences Campus in the heart of the Innovation District in downtown Kitchener, Ontario. The building is also home to the Centre for Family Medicine and the University of Waterloo’s School of Optometry teaching clinic. Students at the Waterloo Regional Campus have the unique experience of living and learning in one of the fastest-growing regions in the country. The Waterloo Regional Campus is situated in Canada’s leading technology ecosystem and students are exposed to cutting-edge advances in medical technology.
| Hamilton Campus Michael G. DeGroote School of Medicine, Faculty of Health Sciences, McMaster University, Michael G. DeGroote Centre for Learning and Discovery, Rm 3101 1280 Main Street West Hamilton, ON Canada L8S 4K1 |
Niagara Regional Campus Michael G. DeGroote School of Medicine, Faculty of Health Sciences, McMaster University, Niagara Regional Campus Cairns Family Health & Bioscience Research Complex, Brock University 1812 Sir Isaac Brock Way St. Catharines, ON Canada L2S 3A1 |
Waterloo Regional Campus Michael G. DeGroote School of Medicine, Faculty of Health Sciences, McMaster University, Waterloo Regional Campus 10 Victoria Street Kitchener, ON Canada N2G 1C5 |
Medicine at McMaster 2022 (PDF) to download this information.
Mission Statement
OUR MISSION
The UGME Program’s mission is “educating and inspiring future physicians to improve health and well-being for all through clinical excellence, innovation, scholarship, leadership and social accountability.”
The core function of the UGME program is to educate future physicians – to provide them with the scientific, professional, and social tools to question, learn, discover and lead consistent with the guiding statement of purpose for the Faculty of Health Sciences.
We inspire so future physicians can join the culture of innovation, exploration and collaboration. We lead the community by example. We provide structure and support to allow our community to learn what was, challenge what is and optimistically embrace what could be.
Health defined by the World Health Organization (WHO) is the “state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.” The Canada Health Act 1985 builds on this “[we] can [improve] … well-being through combining individual lifestyles that emphasize fitness, prevention of disease and health promotion with collective action against the social, environmental and occupational causes of disease, and [we] desire a system of health services that will promote physical and mental health and protection against disease”. It is this calling, to improve overall health and well-being, that we engage and answer as a UGME program.
We align with the World Health Organization’s Towards Unity for Health (Geneva, 2000) endorsing the “Health for All” goal, and the mission to reduce disparities in health and well-being across individuals and groups. This reflects a deep commitment to equity and inclusion, particularly around those who are marginalized and oppressed.
How do we Achieve This?
Excellence in the healthcare environment answers the fundamental regional needs that drive engagement within the UME program. This represents a deep commitment to developing clinical skills and expertise in the service of patients and populations.
Innovation is core to the Faculty of Health Sciences vision and values, and woven within the rich tradition of the UGME program itself. We recognize that innovation represents a deep engagement to defining needs, structures and processes, with the courage to challenge the status quo and the persistence to measure and iterate for productive change.
Advancing health and well-being requires a purposeful, systematic and rigorous approach to discovery, communication and knowledge building. We recognize the central import of scholarly approaches in all core functions and processes of the UGME program.
Leadership is core to the educational and inspirational mission of the UGME program. We foster the development of leadership at all levels, as a key tool to advance our mission, and empower our students and marginalized groups to effect meaningful improvements in health and wellness.
We acknowledge the central role of social and structural determinants on health and wellness. We think deeply on the need to address these determinants to improve the health of the marginalized. We systematically apply an equity and anti-oppression lens to all we do to best address the healthcare concerns of those who are oppressed, under-represented, and marginalized.
Social Accountability Statement
Social Accountability Statement
The UGME program is committed to priority health concerns of the populations we serve: “We commit to serving and including the people and populations in our regions of Hamilton, Waterloo, Niagara, and surrounding communities in all work we do. We reflect systematically with an equity lens on our structures and actions to care, educate, study, innovate and lead in a manner that includes and best serves the marginalized and oppressed.”
The UGME program addresses its social accountability responsibilities through a system of distributed regional campuses and clinical education campuses. This distributed medical education model provides education and clinical experiences within the communities and regions we have a mandate to serve.
The UGME program fosters social accountability through leadership with Chair roles in Diversity and Indigenous Curriculum. The UGME program is committed to recruiting and retaining faculty and administrative leaders, instructors, tutors, facilitators and supervisors who represent marginalized, oppressed, and underserved groups.
The UGME program seeks to address health concerns of all who are marginalized and oppressed, with focused effort on priority groups. Priority groups are identified in a consultative process which considers demographics, healthcare experiences, and needs of groups within the UGME program’s catchment area, revisited biennially by the UGME program executive.
Currently, we identify two groups of priority:
(1) those who identify as Indigenous including First Nations, Métis and Inuit
(2) those who identify with Black ancestry
Expandable List
The UGME program takes a pro-active and longitudinal facilitated approach to supporting priority student populations within the program. This approach recognizes that students from priority groups have unique journeys including facing many barriers and inequities which can slow or impede success. The approach is collaborative involving student affairs, supports (eg. Indigenous Health Learning Lodge, McMaster Black Students Association) and dedicated resources (eg. Indigenous Bursary) focused on each priority group.
Curricular mapping processes are reviewed on a biennial basis by the Curriculum committee and presented at the UGME Executive Committee to identify how priority group health needs are addressed by the curriculum across each relevant component.
The type and location of experiences within the program reflect our social accountability statement, and are reviewed on a biennial basis by the Curriculum committee and presented at the UGME Executive Committee.
Governance
Governance
Like most medical schools in Canada, the Undergraduate Medical Education (UGME) Programs of the Michael G. DeGroote School of Medicine operate consistent with the governance principles and policies of our parent institution, McMaster University. The University Senate is ultimately responsible for oversight of the UGME programs. More information about the Senate, including governance and policies can be found on the University Secretariat page.
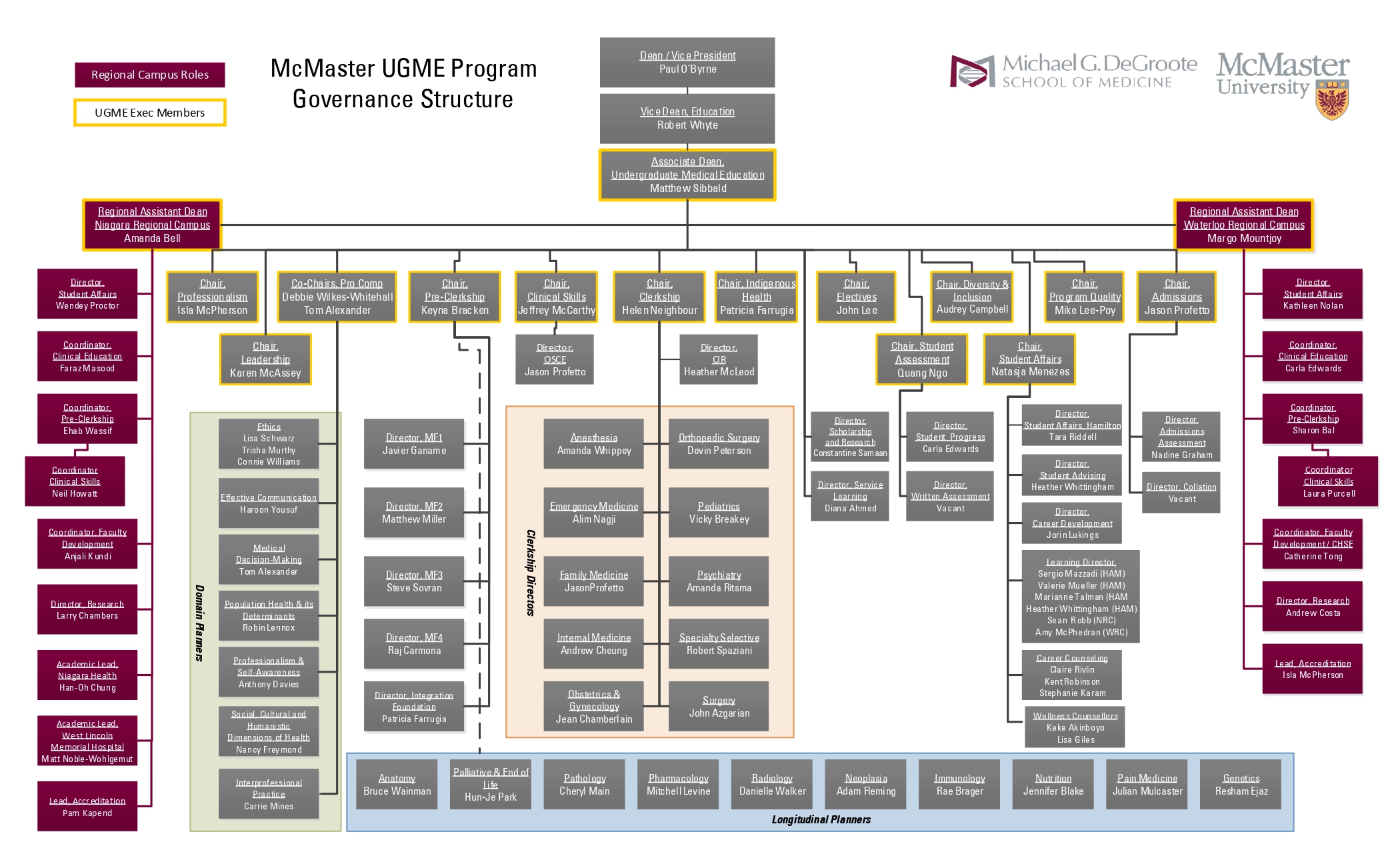
The UGME Program is an educational program offered within the Michael G. DeGroote School of Medicine in the Faculty of Health Sciences. The administrative and governance structures within the Faculty and School of Medicine are provided below.
Expandable List
Governance of the UGME Program is overseen by the UGME Executive Committee which is responsible for direction-setting and policy development for the program. The executive committee includes representation from the following stakeholder groups and portfolio leads (labels borrowed from CACMS[1] accreditation standards and elements): the chief academic officer and chief administrator; the executive leads of each Regional Campus (see Governance of Distributed Medical Education below); admissions; pre-clinical, clerkship, professional competencies, clinical skills and electives curricular components; program evaluation and student assessment; diversity and engagement; and student executive leads (class presidents).
Each of the portfolios listed are led by a Chair who is a faculty leader. Decision-making and activities of each portfolio are coordinated by a committee which may have additional sub-committees where decision-making and work are further delegated. The administrative structure for the delivery of all aspects of the UGME Program is illustrated in the organization(al) chart below.
McMaster’s UGME Program is delivered across three medical education campuses, three additional clinical education campuses and many more affiliated clinical sites. Our three main campuses are the Hamilton Campus (HC) and our two regional campuses, the Waterloo Regional Campus (WRC) and the Niagara Regional Campus (NRC). For additional information about our multi-campus network and additional clinical affiliations, please refer to Mac-CARE or the Regional Campus micro-sites.
Strategic planning, decision-making, and distribution of work across this complex network is accomplished in three ways:
-
Pan-DME committees
-
Multi-site representation on portfolio-based committees
-
Analogous committee structures at different sites
School of Medicine Committees
Council of the School of Medicine
- Regional Assistant Deans are members
- Chaired by the Dean, Faculty of Health Sciences (FHS); includes FHS Associate Deans with portfolios relevant to the School of Medicine, Assistant Deans of the School of Medicine Educational Programs (e.g. UGME, Post-graduate Medical Education, Midwifery, and Physician Assistants), and Chairs of Academic Departments
Distributed Medical Education (DME) Advisory Committee
- Regional Assistant Deans are members
- Chaired by Associate Dean, Education; includes Chair of Department of Family Medicine, Assistant Deans UGME & PGME, Directors of Education Services and Mac-CARE
DME Operations Group
- Regional Assistant Deans, Regional Program Administrators and Clinical Education Coordinators are members
- Chaired by Assistant Dean, UGME; includes representation from Education Services, PGME, Mac-CARE, and Department of Family Medicine
- Meetings are deliberately conducted at each campus throughout the year to enable DME program leadership to review each site.
Undergraduate Medical Education Committees
Executive Committee
- Regional Assistant Deans and Regional Program Administrators are members
- Chaired by Assistant Dean, UGME; includes representation of all Chairs in UGME Program
Deans’ Group
- UGME Assistant Dean and Regional Assistant Deans
Deans’ and Administrators’ Group
- UGME Assistant Dean, Regional Assistant Deans, UGME Program Manager, Regional Campus Administrators
Curriculum Committee
- Pre-Clerkship Coordinators are members
- Chaired by Assistant Dean, UGME
Pre-Clerkship Committee
- Pre-Clerkship Coordinators are members
- Chaired by Pre-Clerkship Chair
Professional Competencies Committee
- Faculty representatives from Regional Campuses
- Chaired by Pro Comp co-Chairs
Clinical Skills Committee
- Assistant Pre-Clerkship Coordinators are members
- Chaired by Clinical Skills Chair
Clerkship Committee
- Clinical Education Coordinators are members
- Chaired by Clerkship Chair
Clerkship Rotation-specific Curriculum Committees
- Rotation-specific Regional Education Leaders are members
- Chaired by rotation-specific Clerkship Director
Clinical Education Committees in each Regional Campus
- Campus-specific Regional Education Leaders are members
- Chaired by campus-specific Clinical Education Coordinator
Academic Progress Committee
- At least one Regional Assistant Dean is present at each meeting
- Includes the Student Assessment Chair, Program Manager, and Curriculum Component Chairs
Curriculum planning, delivery and evaluation are complex, particularly in maintaining appropriate curricular integration and across multiple campuses and other educational sites. A curriculum committee provides central oversight of the curriculum. As with other governance structures included above, the curriculum committee includes multiple stakeholder and portfolio representation. Curricular sub-committees report to the curriculum committee.
Strategic Plan
UGME Strategic Plan
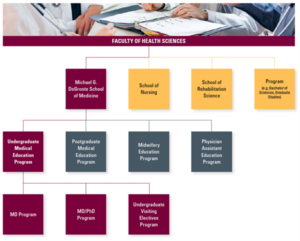
Situating the UGME Program Within the Faculty of Health Sciences
Within the organization structure of the Faculty of Health Sciences, the UGME program is one of four programs in the Michael G DeGroote School of Medicine. It consists of a MD program, MD/PhD program and an Undergraduate Visiting Medical Electives Program.
The undergraduate medical education (UGME) program engages in an ongoing planning and continuous quality improvement process that establishes short and long term programmatic goals using a process outlined in the Strategic Planning Process document. This process is focused on the achievement of measurable outcomes that improve programmatic quality, and ensures effective monitoring of the program’s adherence with accreditation standards.
This strategic plan was generated through a four stage process which included: surveying, leadership consultation, focus groups and committee vetting.
Our Strategic Priorities Include:
DOMAIN 1: EDUCATE AND INSPIRE to the highest level of competence, capacity and professionalism
Graduate competent and capable future physicians instilled with McMaster values to lead in the delivery of healthcare and be emissaries of its international reputation.
| SHORT TERM GOALS | LONG TERM GOALS |
|---|---|
| Maintain a widely accessible map of UME curriculum and assessment linking and aligning each activity to one or more core curricular objectives. Provide and reference these maps to students, staff and faculty within each core curricular unit.
Renewed focus on professionalism: b. Update the Professionalism in Practice rubric outline professional expectations in collaboration with the School of Medicine c. Create a UME Professionalism policy to streamline report, feedback and management of professionalism concerns Clinical skills development. Create opportunities within each clinical skills foundation unit to provide formative assessment organized to prepare students to achieve the AFMC Entrustable Professional Activities Enhance service learning: create a Director of Service Learning role to structure, support and engage students in service learning opportunities |
Longitudinal career exploration program: develop and implement a longitudinal program within the pre-clerkship leveraging virtual and online platforms to expose students to a “day in the life” of different physician types
Longitudinal professional development portfolios: provide structure, support and recognition on student transcripts for systematic engagement in leadership, scholarship, and service learning. Build a portfolio process and assessment system with metrics around objectives, professional development, engagement, dissemination, and reflection Integrate AFMC Entrustable Professional Activities systematically throughout the curriculum to facilitate the development of key professional competencies, and incorporate their assessment within the transition to residency Ongoing systematic program evaluation and establishment of continuous quality improvement focused on a subset of accreditation standards in rotation each year
|
DOMAIN 2: SOCIAL ACCOUNTABILITY
Excel in our mission of distributed medical education to address priority health concerns of the community and region we have a mandate to serve, while upholding our Faculty of Health Science values of equity, diversity, and inclusion.
| SHORT TERM GOALS | LONG TERM GOALS |
|---|---|
| Identify priority health concerns of groups identified within the social accountability framework: implement a scoping process to identify priority health concerns and report these to UME leadership and community on biennial basis
Establish and support a Chair of Indigenous Curriculum in collaborative allyship with the Faculty of Health Sciences’ Indigenous Health Initiative Admit and retain Black students as an identified priority group: Establish a direct-application stream for Black students and provide support for their success within the program Address priority health concerns of groups identified within the social accountability framework throughout the curriculum, and make this transparent through accessible curricular and assessment maps: maintain a curricular map which identifies areas of the curriculum, types and locations of experiences which address priority health concerns of groups identified within the social accountability framework |
Increase scholarship and bursary funding: support students in financial need with a focus on students from marginalized and underrepresented groups
Measure diversity within the program: conduct annual surveys of students, staff and faculty, summarized for program leadership and the broader community Measure success of addressing health concerns of priority groups identified within the social accountability framework: establish and measure outcomes related to social accountability on an annual basis |
DOMAIN 3: LEARNER EXPERIENCE
Focus on the student journey, emphasizing the importance of autonomy, resilience and wellness.
| SHORT TERM GOALS | LONG TERM GOALS |
|---|---|
| Optimize communication between students and program leadership: Create a staff role dedicated to communications to streamline townhalls, coordinate electronic newsletters and online information updates.
Facilitate the reporting and handling of student mistreatment concerns: Streamline process for reporting mistreatment, and streamline the downstream processes for managing mistreatment concerns. Develop leadership mentorship program to support those involved in student leadership through a longitudinal structured program focused on development of leadership knowledge, skills, and identity. Update assessment and appeal policies: renewed focus on transparency and empowerment of learners in understanding assessment standards and processes, and ensuring alignment and clarity with University processes for appeal. Wellness: Expand flex day policy to create opportunity for a flex day in each Medical Foundation. |
Support the improvement of the learning climate: foster a programmatic approach to improving the learning climate with ongoing assessment of the learning climate and site reviews every 3 years. Review mistreatment concerns in an integrated model with postgraduate medical education. Develop processes of support to measure, change, and monitor the learning climate.
Foster resilience and wellness in the curriculum: Systematically integrate wellness and resilience training strategies within the core curriculum throughout the program Online accessibility: Overhaul the external web page with paths catering to different user types to provide transparent access to descriptive information, resources and policies. Highlight successes of students, staff and faculty through social media and web based strategies.
|
DOMAIN 4: LEAD THROUGH RESEARCH AND INNOVATION
Foster research and innovation by students, faculty and leaders. Innovate with a continuous quality improvement lens, using a scholarly lens to engage internationally as a leader in undergraduate medical education
| SHORT TERM GOALS | LONG TERM GOALS |
|---|---|
| Build scholarship opportunities: Expand and maintain a distributed model of research and scholarship opportunities such that every student can engage and meaningfully contribute to structured scholarly activities that fit within the three year program, with defined and tracked outcomes.
Scholarly scoping consults: partner with the educational scholarship community (e.g. MERIT, Clinician Educator Diploma Program and the Health Sciences Education Masters Program) to provide high-level summaries of relevant educational theory and evidence around proposed program policy, process or curricular changes, with a dual purpose of equipping faculty leaders and decision makers with robust evidence for decisions while supporting scholarly approaches to knowledge synthesis Foster scholarship in distributed medical education that builds regional, national, and international collaborations focused on defining and measuring processes, policies and outcomes.
|
Modify curricular review to incorporate continuous quality improvement cycles: build continuous quality improvement cycles within the curricular committee review work to iteratively improve curricular components
Collaborate internationally with other 3 year undergraduate medical programs to share, innovate and report on educational process and outcomes to optimize programming for a three year program format Build and support partnerships with regional clinical and academic centers of excellence that foster service, leadership and clinical opportunities for students to accelerate their professional growth |
DOMAIN 5: ENGAGE AND CONNECT FOR RESILIENCE AND GROWTH
Engage and connect within our program, departments, university and healthcare community to enhance and support our UME mission while ensuring resilience and sustainability of the program
| SHORT TERM GOALS | LONG TERM GOALS |
|---|---|
| Leadership development for faculty and staff: provide at least one focused relevant leadership development opportunity for both program leaders and staff each year
Align affiliations with accreditation standards: Renew all Hospital affiliation agreements to ensure ongoing alignment of affiliations with accreditation standards. Decentralize core curricular components: Adopt a model for large group sessions which uses either virtual or concurrent curriculum presentation at distributed sites Asynchronous document consultation process: take advantage of the full potential of cloud-based document sharing to develop, consult and approve processes, policies and documents wherever possible. Use asynchronous approval processes without meeting wherever possible. Aim for all documents to be circulated two weeks in advance for asynchronous comments before meetings. Optimize meetings: Regular review of committee terms of reference with attention to minimize meeting burden, meeting frequency, meeting participants, travel time ratio using virtual platforms, pre-circulated agendas and documents, point form minutes, and cloud based documents storage. |
Update electronic records platform: Migrate to an updated version of Medsis that tracks accommodations, student absences, and alternate training paths.
Connect regularly with staff and faculty: Maintain a staff, faculty and leadership database. Build links to the faculty group through an annual meeting, annual report, and surveys to proactively identify challenges. Build and maintain relationships with clinical departments and hospital partners: Provide an annual report, and present once every three years for major stakeholders (Clinical Chairs, regional Hospital meetings) Optimize resourcing of program leaders: Adopt a central process for review of all job descriptions with each posting and renewal to include sections containing expectations around staff support collaboratively developed with program administration, professional development support, accreditation accountability collaboratively developed with the Chair of Program Evaluation.
|
MACcred2023
MACcred2023
The McMaster University, Michael G DeGroote School of Medicine, Undergraduate Medical Education program is currently undergoing accreditation, a comprehensive review overseen by the Committee on Accreditation of Canadian Medical Schools (CACMS).
This process evaluates the quality of our program to ensure we are providing our students with the right skills they need to serve our communities as future physicians. We’re listening to students, talking to staff and faculty, and doing everything we can to ensure our med students continue to get one of the best educations in Canada!
What is accreditation?
Every eight years, medical schools in Canada carry out a comprehensive review of their educational quality to ensure compliance of accepted standards set out by the Committee on Accreditation of Canadian Medical Schools (CACMS). Medical schools provide reviewers with written submissions to demonstrate compliance, and reviewers also meet virtually and in-person with medical school faculty, students, and staff.
The Undergraduate Medical Education program was last accredited in May 2015. Accreditation is a multi-year process that wouldn’t be possible without the hard work and participation of our staff, our faculty, and our students. We want to thank everyone involved for all of their support!
Why is accreditation important?
Accreditation through CACMS provides assurance to everyone in healthcare and the public that our program properly prepares our students with the skills they need for the next stage of their training.
This process ensures that McMaster UGME’s:
- educational programs culminating in the award of the M.D. degree meet reasonable, generally-accepted, and appropriate national standards for educational quality, and
- graduates of such programs have a complete and valid educational experience sufficient to prepare them for the next stage of their training
Check out the CACMS website for more information.
2023 Accreditation Timeline
Accreditation is an extensive process involving several key steps that span multiple years.
There are seven steps to the overview process:
Expandable List
The UGME program and the CACMS Secretariat establish the dates for the virtual and in-person site visits, and the CACMS Secretariat sends the UGME program the materials and instructions for completing the accreditation process.
Coordination for the upcoming accreditation has been ongoing since Spring 2021, and the site visits will take place in Spring 2023.
UGME faculty and staff members contribute information (ex. statistics; policies; initiatives; outcomes) to the Data Collection Instrument (DCI), a CACMS document that collates medical school data relating to the accreditation standards. An important contribution to the DCI is the Independent Student Analysis, survey data generated by the undergraduate medical students that helps to demonstrate the impact of the medical school’s educational efforts.
Information for the DCI was primarily compiled in late-2021 and early-2022; however, the UGME program has opportunities to update information in the DCI until January 2023.
Groups of UGME faculty members, staff members, and medical students collectively use information from the DCI to evaluate the UGME program against the accreditation standards. The narrative evaluation responses are entered into the Medical School Self-Study (MSS), a CACMS document that collates and maps these responses in relation to the accreditation standards.
Responses for the MSS were composed in Spring 2022 and reviewed by faculty leadership in Summer 2022. The UGME program has opportunities to update information in the MSS until December 2022.
The UGME program submits the finalized MSS and DCI to the CACMS Secretariat, which in turn distributes these files to the external faculty members making up the visit team for the UGME program’s 2023 accreditation. The visit team reviews these materials in preparation for the site visits.
The CACMS visit team conducts site visits to “verify and update information compiled in the school’s DCI, clarify any issues that are unclear, view the environment and facilities for learning first-hand, and meet with administrators, faculty members, and students. The team will meet with the dean to explain its purpose and gain input in a conference at the beginning of the site visit, and meet with the dean and campus chief executive to summarize its findings about the program’s strengths and areas of noncompliance at the completion of the visit. The visit process, the appointment of visit teams, visit report, and documents considered by CACMS in reaching accreditation decisions are explained in the CACMS Rules of Procedure.” – CACMS
The CACMS visit team secretary collates the written findings of each visit team member into “a visit report that describes the program of education and accounts for the school’s compliance with each of the standards of accreditation as contained in the CACMS Standards and Elements. The preparation, review, and processing of visit reports, and the information considered for accreditation determinations are given in the CACMS Rules of Procedure.” – CACMS
“CACMS bases its accreditation determination on the visit report, supplemented as necessary by information contained in the DCI and the institutional self-study. Details of the deliberations of CACMS, acceptance of evidence, consideration of progress reports, and reporting of decisions are found in the CACMS Rules of Procedure.” – CACMS
Below you can find a high-level critical path for our work as well as a breakdown of the workflow:
For More Information
If you have any questions about accreditation, please contact:
- Mike Lee-Poy, Chair of Program Quality, Michael G. DeGroote School of Medicine
- Mike Weir, Program Coordinator, UGME, Michael G. DeGroote School of Medicine
